In the world of physical therapy, meticulous documentation is paramount for tracking patient information, monitoring progress, and ensuring effective communication among healthcare providers. One highly effective method for achieving these objectives is through the use of SOAP notes for physical therapy.
Today, in this blog post, we will delve into the origins of SOAP notes and provide a step-by-step guide on how physical therapists can effectively utilize this documentation method to optimize patient care.
Let’s delve deep into this.
What is SOAP Notes for Physical Therapy?
SOAP, an acronym for Subjective, Objective, Assessment, and Plan, represents a structured and comprehensive approach to documentation that facilitates both interdisciplinary and intradisciplinary care. This method is indispensable for physical therapists as it ensures that detailed patient progress is consistently recorded and easily accessible within medical records.
These notes detail the entire interaction between a therapist and a patient, capturing the initial information gathering, formulating hypotheses about care, and determining the most effective diagnosis and plan of care (POC) based on the collected data. Essentially, SOAP notes track the patient’s journey from intake through discharge.
SOAP notes not only streamline communication among healthcare providers but also enhance the Clinical Reasoning process, aiding therapists in collecting information, formulating and testing hypotheses, and determining the most effective diagnosis and treatment plans.
In physical therapy, SOAP notes have gained popularity for their clear, organized approach to tracking patient care and for guiding other treatment providers, while also meeting legal documentation requirements for insurance purposes.
Experience live demo and create customized SOAP notes for Physical Therapy.
How to Effectively Write PT Soap Notes: Step-by-Step Guide
A pt SOAP note example is essential for maintaining detailed records, ensuring accountability, and enhancing communication with other healthcare providers.
Using Electronic Medical Record (EMR) software with advanced note-taking and data management features can significantly improve the efficiency of documentation.
- SOAP Note Subjective:
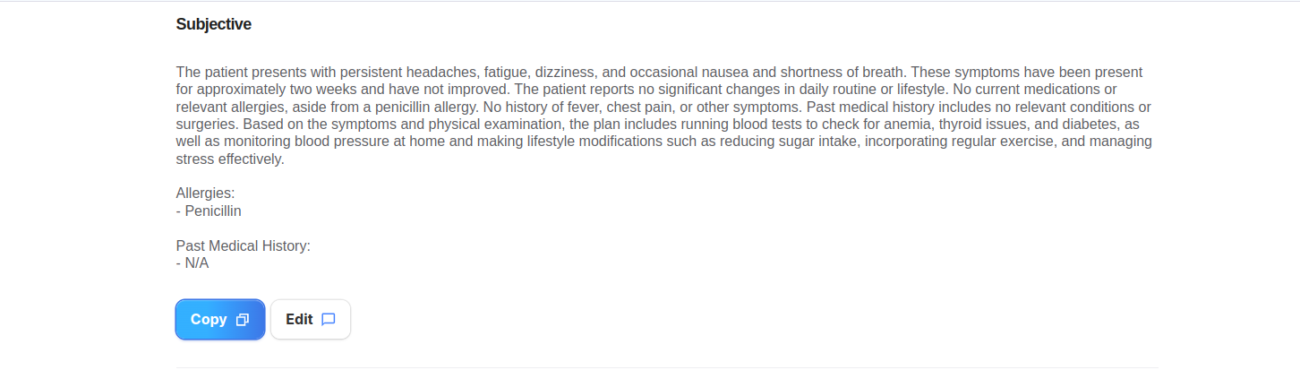
The term ‘Subjective’ refers to the first section of a pt SOAP note, which reflects the patient’s personal feelings and opinions. This part provides a comprehensive account of the patient’s experiences from their perspective, including their current condition, symptoms, activity level, family history, and more.
In the Subjective section, the focus is on capturing the patient’s view of their functional status, such as:
- Their perception of how treatment is progressing
- Their current level of function and any changes observed
- How their quality of life is improving
- Their thoughts on overcoming their condition
This section should also include relevant medical details from the patient’s chart if not directly observed by the therapist, as well as information from family members or caregivers. Direct quotes from the patient or their family should be enclosed in quotation marks when discussing treatment intervention.
- SOAP Notes Objective:
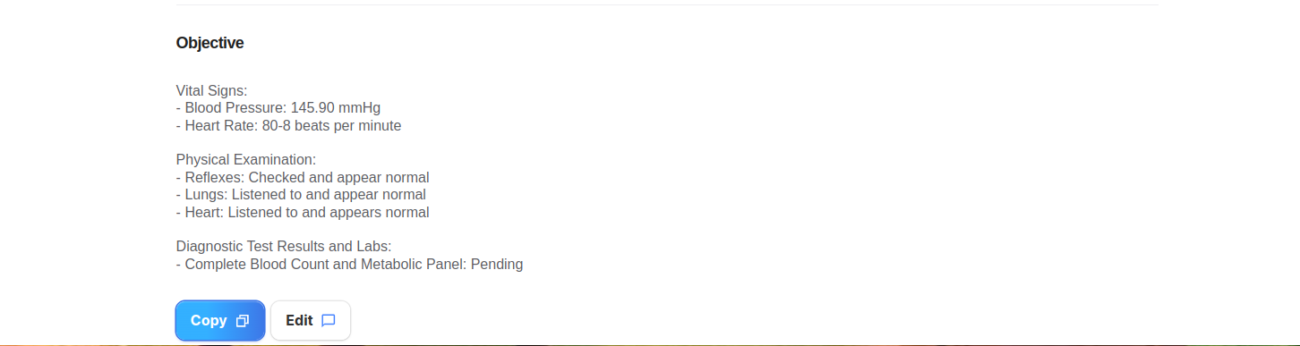
The next stage in writing SOAP notes is the ‘Objective’ section, which is crucial for documenting observable data and treatment specifics. In this part, therapists should include precise measurements such as range of motion and vital signs, along with details of treatment interventions, including:
- Frequency
- Duration
- Equipment used
Although the Objective section may not carry as much legal weight as other parts, it plays a significant role in patient care. It provides a clear, measurable record that enables any other healthcare professional to understand and continue the patient’s treatment seamlessly.
Unlike the Subjective section, which is based on personal experiences, the Objective section relies on factual, quantifiable observations. It should detail activity limitations, participation restrictions, and impairments in body structure and function. This approach helps track patient progress accurately and assess the effectiveness of treatment over time.
- SOAP Notes Assessment:
The “SOAP Assessment Physiotherapy” section captures the physical therapist’s rationale behind the recommended treatment plan. This is the most crucial legal note, particularly for insurance and Medicare compliance, as it meets the therapist’s legal duty to document patient progress. It should detail the reasoning behind both the diagnosis and the treatment.
An Assessment section encapsulates the analytical thinking involved in problem-solving, including:
- The ultimate goals of treatment
- How subjective and objective findings influenced the treatment plan
- Why the treatment is specifically suited to the patient’s condition
- Factors that could impact treatment goals and how to address them
This section should expand with each care episode, providing a space for the therapist to record their professional assessment of each session. Updates should include patient progress towards goals and any positive or negative responses to the treatment.
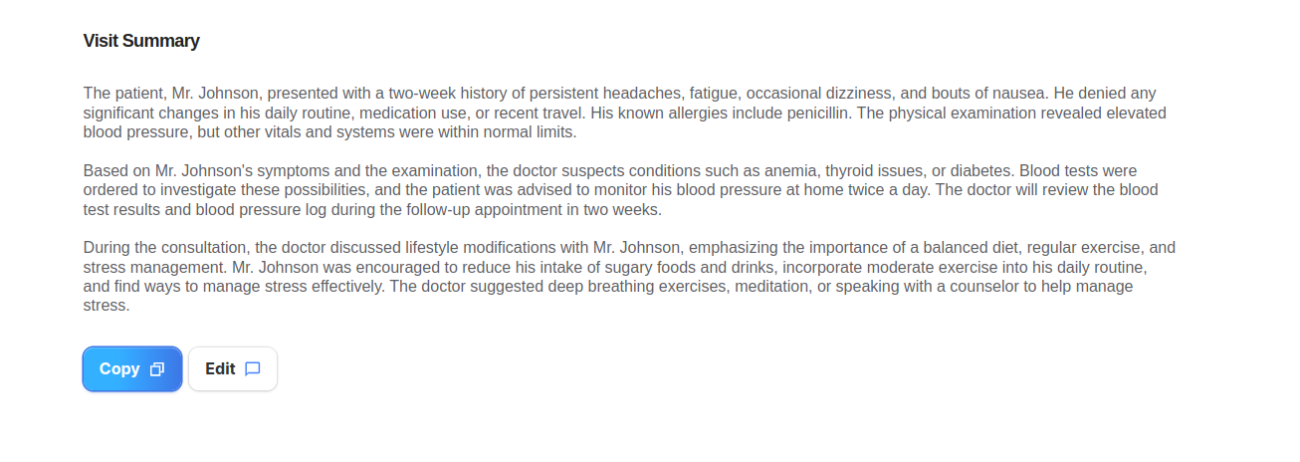
- SOAP Notes Plan & Visit summery:
The final step in writing SOAP notes involves outlining the patient’s future treatment plan. This section should detail your planned actions for upcoming sessions, including any new treatments and patient assignments to complete before the next visit.
Instead of merely stating “continue with treatment” even if the plan remains unchanged, provide specific details about what will be addressed. Detailed SOAP notes are crucial for both your benefit and that of the patient’s care team, ensuring clarity and continuity in care.
Additionally, if you plan to adjust the treatment strategy, use this section to document those modifications. This ensures that any changes are clearly communicated and recorded.
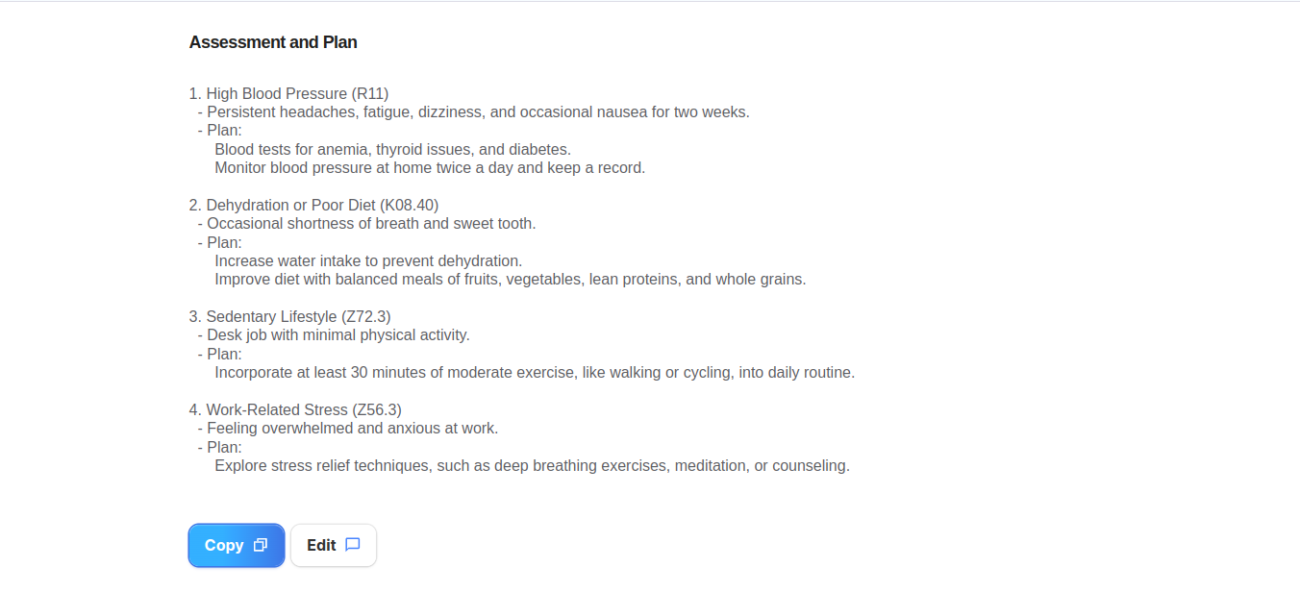
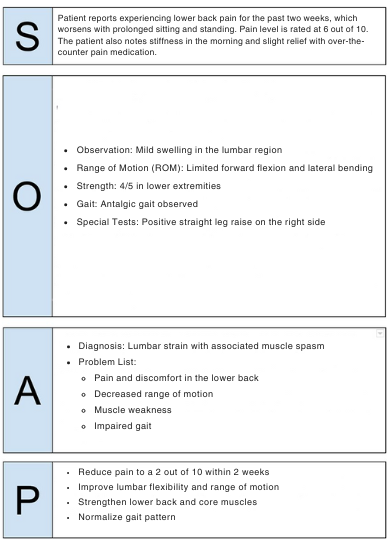
A SOAP Note for Physical Therapy Examples
Here is a detailed pt SOAP note example mentioned below:
Subjective (S): Patient reports experiencing lower back pain for the past two weeks, which worsens with prolonged sitting and standing. Pain level is rated at 6 out of 10. The patient also notes stiffness in the morning and slight relief with over-the-counter pain medication.
Objective (O):
- Observation: Mild swelling in the lumbar region
- Range of Motion (ROM): Limited forward flexion and lateral bending
- Strength: 4/5 in lower extremities
- Gait: Antalgic gait observed
- Special Tests: Positive straight leg raise on the right side
Assessment (A):
- Diagnosis: Lumbar strain with associated muscle spasm
- Problem List:
- Pain and discomfort in the lower back
- Decreased range of motion
- Muscle weakness
- Impaired gait
Plan (P):
- Treatment Goals:
- Reduce pain to a 2 out of 10 within 2 weeks
- Improve lumbar flexibility and range of motion
- Strengthen lower back and core muscles
- Normalize gait pattern
- Interventions:
- Modalities: Apply heat therapy for 15 minutes followed by electrical stimulation for 10 minutes
- Manual Therapy: Perform soft tissue mobilization and lumbar traction
- Exercises: Prescribe core strengthening exercises, lumbar stabilization exercises, and gentle stretching
- Education: Instruct the patient on proper body mechanics and posture
- Home Exercise Program (HEP): Provide a tailored set of exercises to be performed daily at home
- Follow-Up: Re-evaluate the patient in one week to assess progress and adjust the treatment plan as needed.
To get a complete hold on how to generate SOAP notes for Physiotherapists, read this SOAP Note Generator in 2024.
The Bottom Line
Effectively writing SOAP notes is essential for physical therapy to ensure accurate documentation and optimal patient care. By incorporating RevMaxx AI Medical Scribe into your practice, you can further enhance your documentation process.
We offer advanced AI-powered tools that streamline note-taking, improve accuracy, and reduce administrative burdens. Its features like voice-based workflows and automated ICD-10 coding ensure over 95% accuracy and compliance, making it easier to create detailed SOAP notes efficiently. Enhance your clinical documentation with RevMaxx and focus more on patient care.